This major study in public hospitals in NSW[7] compared the psychosocial matched care approach applied in some hospitals (intervention group) to those who had usual care (control group).
Table 1 shows the lost workdays, claims costs and expected future cost trajectory of those identified as having elevated psychosocial risk. It compares the results of the psychosocial matched care system on those with elevated risk ratings within intervention hospitals with those at control hospitals that followed usual care.
Table 1 - WISE study intervention vs control group outcomes
Metric |
Intervention Group |
Control Group |
Lost workdays (at 24 months post-injury) |
31.7 days |
66.5 days |
Claims cost (at 24 months post-injury) |
$16,443 |
$23,405 |
Cost trajectory |
Costs tapered off and stopped by 30 months |
Significant ongoing costs |
Figure 1 shows the claims costs by month, comparing those at elevated risk who were managed by usual care (control group) or those who were managed with early psychosocial matched care.
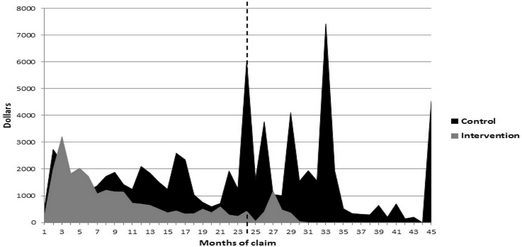
Figure 1 - Claims costs per month comparing intervention and control groups in those with elevated risk
Psychosocial outcomes
After receiving targeted support the high-risk workers' psychosocial screening questionnaire scores (ÖMPSQ-SF1) improved significantly, moving from the high-risk range (average score of 58.9/100) to the low-risk range (average score of 35.4/100). This change was statistically significant and also large enough to be clinically meaningful. Importantly, their lost time outcomes approached those of the low-risk cohort.
Significant improvements in psychosocial measures were noted:
•Distress levels (measured by the DASS) decreased substantially.
•Disability levels (measured by the BPI) decreased notably.
•Pain self-efficacy (measured by the PSEQ) improved significantly, with average scores increasing from 33.1 to 45.8 (a level associated with the ability to work despite persisting pain)
•Pain-related distress (measured by the Pain Catastrophising Scale) showed a large improvement, even though the initial scores were not very high.
These results demonstrate that the psychosocial matched care system reduced the psychosocial risks, with improvement across all the measured psychosocial domains.